2024 Yale NEA-BPD Research Conference
Presentation
Compass Research Poster
A Deeper Dive
Treatment History of Participants (2023 Residential Admissions)
Prior Hospitalization (24+ hours)
- 23.1% (n=6) had ZERO hospitalizations prior to admit
- 38.5% (n=10) had a single hospitalization prior to admit
- 31% (n=8) had between 2 and 5 hospitalizations prior to admit
- 0.04% (n=1) had 10+ hospitalizations prior to admit
Prior RTC
- 50% (n=13) had no RTC stays prior to Farmhouse Admit
- 34.6% (n=9) had 1 RTC stays prior to Farmhouse Admit
- 11.5% (n=3) had 2 RTC stays prior to Farmhouse Admit
- 3.9% (n=1) had 3 RTC stays prior to Farmhouse Admit
Measures
RTC Assessment Battery
(Intake & Discharge)
PHQ-9 / A
The Patient Health Questionnaire for Adolescents is a self-report questionnaire for diagnosing and screening for depression in adolescents.
GAD-7
The Generalized Anxiety Disorder-7 is a self-report questionnaire for assessing the severity of Generalized Anxiety Disorder Symptoms.
BRFL-A
The Brief Reasons for Living Inventory for Adolescents is used to identify protective themes in a suicidal individual’s life.
BSL-23
The Borderline Symptom List is a self-report questionnaire used to assess the severity of Borderline Personality Disorder Symptoms in adults.
DBT-WCCL
The Dialectical Behavior Therapy (DBT) Ways of Coping Checklist is a self–report questionnaire used to identify how individuals use DBT skills in their daily lives.
DERS-SF
The Difficulties in Emotion Regulation Scale Short Form is a self-report questionnaire used to assess emotion regulation problems in adults.
PCL-5
The Post-traumatic Stress Disorder Checklist for the DSM-5 is a self-report questionnaire for assessing PTSD severity.
SCIM
The Self-Concept and Identity Measure is used to assess identity-related dysfunction and distress.
SCS
The Self-Compassion Scale is a self-report questionnaire used to assess an individual’s capacity for self-compassion.
SCORE-15
The Systemic Clinical Outcome and Routine Evaluation is a self-report questionnaire used to measure family functioning and change.
PHQ-9 / A
The Patient Health Questionnaire for Adolescents is a self-report questionnaire for diagnosing and screening for depression in adolescents.
GAD-7
The Generalized Anxiety Disorder-7 is a self-report questionnaire for assessing the severity of Generalized Anxiety Disorder Symptoms.
Weekly RTC Assessments
Family Programming Information
DBT Multi-Family Skills Training Group
Participation in a truncated version of DBT Multi-Family Skills Training Group is required of all families who are admitted to the RTC. Instead of the 16–24-week group schedule outlined by Rathus & Miller, our program has pared the material down to 10 lessons (1. Introduction to DBT, DBT Assumptions, Goals of Skills Training, 2. Dialectics, 3. Validation, 4. Principles of Behavior Change, 5. Mindfulness, 6. Crisis Survival Skills, 7. Reality Acceptance Skills, 8. Understanding and Naming Emotions, 9. Changing Emotional Responses, and 10. Interpersonal Effectiveness). Multi Family Group follows the same format as the one proposed for outpatient DBT-A: Mindfulness practice, homework review, presentation of new material, and assigning homework (behavioral rehearsal and worksheet completion). The group is didactic in nature (not a process group) and skills are presented in the context of family functioning.
Caregiver Consultation Group
A weekly “caregiver consultation” group is attended by caregivers only and serves several functions; clarifying concepts taught during Multi Family Skills Training Group, providing a non- judgmental environment to discuss the unique experience of raising a suicidal adolescent, facilitating validation and encouragement among participants, informal exposure to trauma-related cognitions, emotions, etc. associated with the adolescent’s life-threatening behavior, and trouble-shooting scenarios that are likely to occur post-discharge. Of specific importance is identifying and troubleshooting the barriers to caregiver follow-through with Parent Response (Contingency Management) Plans. This is a space where intergenerational patterns of attachment are often discussed, as attachment style and beliefs about adolescent-caregiver relationships are often barriers to effective engagement in the treatment. Each Caregiver Consultation group ends with a Mindful Self Compassion that is believed to mitigate the impact of post-traumatic stress.
Attachment-Based Family Group
“Attachment-Based Family Group” combines concepts of attachment theory (secure base, attunement, differentiation, separation distress, etc.) with DBT skills and principles. An attachment concept is presented briefly, followed by an experiential activity that explore attachment styles, ruptures, transactions, and repairs. Activities also promote adolescent-family connections, effective communication, emotional vulnerability, and cultivating a positive family identity.
Adolescent-family connection is promoted by the collaborative identification of activities that provide opportunities for neutral to positive experiences together. Families improve communication through the utilization of a “speaker-listener” script which promotes non-blaming identification of problems, the identification and communication of emotional impact, and behaviorally descriptive requests for change. Emotional vulnerability is achieved via shared exploration of internal experiences of emotions and family identity is promoted through the identification of shared family values and priorities.
Family Therapy
Family therapy occurs twice per week with sessions lasting up to 90 minutes. Sessions are modeled after Alan Fruzzetti’s DBT Family Therapy training and have an emphasis on identifying and repairing attachment ruptures using interventions from Attachment-Based Family Therapy and Emotionally Focused Family Therapy.
What Parents are Saying…
The parent group gave me an instant support system and I didn’t realize that I needed that. A safe place to talk about concerns with no judgement. Everyone understood.
Having the parents involved in the Weekly (Saturday) sessions is critical to the success in our opinion – This allowed the parents to interact and understand the skills being used/taught/shared so that we could better understand and look through a different lenses to better understand the struggles our kid was going through and how to address those differences in ways we would have never thought of or been taught in local groups or treatments that we had found.
The best thing about my daughter’s time in the farmhouse was the hours of family therapy and multiple opportunities for parents to be involved and learn DBT skills. Other programs do not compare in this regard. Every professional was extremely knowledgeable and empathetic.
(In response to “What was effective or helpful about Saturday Family Programming?): Making sure that parents/kids were receiving the same training. Having the group setting to allow everyone to see what challenges they had in common – we’re not alone in this – and to support each other.
Finally, another critical component of the program is Compass’ family wholeness focus and the opportunities to engage, learn DBT, and participate in family days. This really sets Compass apart from any other program I found. Because I’ve had the opportunity to learn and practice DBT skills throughout my child’s stay at the Farmhouse, I think it unlikely that my child will seriously relapse. And, we have the skills we need to better communicate, express emotions in a healthier way, handle minor setbacks and we have improved our relationship.
The parent support group really stood out to us as we haven’t had that level of support, community and sharing before. Loved it.
Floor Staff Training
Floor staff or “Guides”, commit to a 24-month DBT Training Externship. Externship opportunities require either 1) current enrollment in a graduate school program on track to become a mental health professional, or 2) completion of a bachelor’s degree with the intent to apply to a graduate program to become a mental health professional. Our residential program is a “therapist incubator”, providing student clinicians with the opportunity to:
- Co-facilitate clinical groups: DBT, CBT, Mindfulness, Self-Compassion, ACT, Executive Functioning. A licensed clinician is present and a scoring rubric is utilized to give feedback and to assist the student clinician to develop mastery.
- Receive intensive training in evidenced-based treatments that inform our milieu management protocols, such as: DBT & CBT Foundational Training, Behavioral Therapy, ERP, Family-Based Therapy for AN, CBT for Insomnia, MED-DBT, RO-DBT.
- Many of our Guides choose to do their clinical practicum hours in our residential program, allowing them to co-facilitate: DBT-MFG, PET, and Attachment Based Family Group, in addition to weekly group curriculum.
Guides attend 1 hour a week of DBT Skills Group, or a related training topic such as ED Protocols, etc. DBT Skills Group focuses on a Guide’s own skills knowledge acquisition and personal skills use.
Guides attend 1 hour a week of Consultation Team where clinical consultation questions are discussed and answered as an entire team across shifts. Practicum Students attend an additional 2 hours a week, participating in a DBT Training Consultation Team.
In a unique opportunity, Guides are given a direct clinical supervisor ( a licensed clinician), that provides weekly clinical supervision. Assigned readings are reviewed, weekly DBT skills HW assignments are reviewed, and clinical consultation questions pertaining to DBT skills coaching in the milieu are discussed. This is also a time where clinical role plays are focused on for feedback and mastery.
Guides are compensated 4 remote hours a week to:
- Complete weekly DBT core text reading assignments
- DBT For Dummies, by Gillian Galen and Blaise Aguirre
- DBT Skills Training Manual, by Marsha Linehan
- DBT Skills Training for Adolescents, by Jill Rathus and Alec Miller
- Chain Analysis in Dialectical Behavior Therapy, by Shireen Rizvi
- Phone Coaching in Dialectical Behavior Therapy , by Alexander Chapman (adapted for milieu coaching)
- Attend clinical supervision
- Attend weekly Farmhand Meeting were clinical consultation questions are discussed and answered as an entire team across shifts
- Attend weekly Guide DBT Skills group
Skills Deficit Model
Our skills deficit model reduces stigma and blame by taking a non-judgemental stance, with a focus on assessing for missing skills.
- We use a robust individual and group reinforcement and contingency management system to decrease therapy interfering / egregious behaviors and increase skillfull behaviors.
Agreements
Before admission, Compass reviews the following agreements with residents and caregivers and obtains a strong commitment to these agreements as a condition of admission.
Resident’s Agreements
- Psychological Safety: We agree to come together to create an emotionally safe environment that fosters healing. Residents are to be mindful when sharing struggles with target behaviors in a peer group setting. Residents agree to not provide details or in-depth discussions with peers about target behaviors:
- Target behaviors are ineffective ways of coping with emotional pain, such as substance abuse, self-harm, eating disorder behaviors, suicide thoughts and actions, risky and impulsive sex, etc.
- If wanting to share in group or with a peer that you are struggling with urges, please say: “I am struggling with urges to engage in my target behavior(s).” You will get the support you need and be highly reinforced for your mindfulness to others.
- STAT: Stop Talking About That. If a resident starts talking about a target behavior in detail, they will be reminded to be effective with a verbal reminder of STAT and be redirected to say, “my target behavior.”
- Therapeutic Programming: On the one hand, we ask that residents agree to work toward their life worth living by participating fully in treatment. On the other hand, working toward one’s goals is hard work and the road to recovery can often take the form of “two steps forward, one step back.” To balance these two points, a middle ground is the freedom to do one’s best. As you work on your goals and attend programming, strive for full success (i.e., throwing yourself into the program and the skills we will teach you), while at the same time, giving yourself the same grace that we will demonstrate during the times the things you struggle with appear. If we hold both these positions to be true, then that will give you the freedom to do your best at all times – try new things, take risks, and give yourself lots of room for trial and error as you learn to apply skills on the path toward your life worth living.
- Skillfulness: Residents agree to practice all the skills they are taught, ask for skills coaching from Guides when they are struggling, and to practice opposite action and turning their mind towards willingness when they are feeling willful.
- Pro-Skills Culture: Residents make a commitment to not idealize and attempt to connect around depression and other self-destructive behaviors. Residents agree not to discourage effective skills use amongst peers. Residents agree to cheerlead each other’s emerging skillfulness and bond around a compassionate response to the journey and the joy and community that happens through developing mastery.
- A Trauma Informed Culture: Residents agree to practice mindfulness to others. Some of our residents have experienced traumatic events in their life. Residents agree to be effective and mindful of conversation topics as some can be a cue for traumatic events (i.e., topics of a sexual nature, verbal aggression, physical aggression, gossip, etc.). Residents agree that if urges arise to engage in topics of conversation or behavior that can be a cue for traumatic events, they will use skills or ask a guide for help. For example, if anger a guide may suggest the resident to go to the gym with a Guide and use exercise to regulate emotions.
- Target Behaviors: Residents agree to ask for skills coaching from Guides PRIOR to engaging in a target behavior. If a resident engages in a target behavior, they commit to completing a behavioral chain analysis with a Guide, identifying the missing skill, and fully practicing this skill.
- Relationship Repairs: When entering our community, residents agree to practice the skill of “Repair & Overcorrection” when their unskillfulness has damaged a relationship. This involves taking responsibility for their behavior, genuinely apologizing to the person(s) impacted by the behavior(s), and over-practicing the missing skill that led to the breach of trust.
- Inclusive, Dialectical, and Non-Judgmental: Residents agree to practice the principles of inclusivity with peers. Respecting pronouns, being mindful to be socially inclusive of all residents, practicing perspective taking, and committing to taking a non-judgmental stance. In practice, this might look like hearing an awareness creating “ding” of the singing bowl and being asked to replace using the word “but” with “and” or rephrasing a judgmental statement into a non-judgmental statement.
- Healing First: Residents agree to focus on their own healing and recovery. There will be no private relationships (i.e., dating, flirting, intimate talk, etc.) while in program. Residents will also focus on their own recovery and allow other residents to do the same. Focusing on another resident’s recovery prevents residents from focusing on their own healing and prevents potential skill development for both residents.
- Limits: Residents agree to respect the limits of staff and fellow residents by staying mindful of their relationship to staff and fellow residents. Examples of this would include not speaking on behalf of another resident but encouraging them to accurately communicate, not going into a peer’s room and only entering a staff room with permission and accompanied by a staff, or not touching staff or peers without asking their permission first. Residents agree to observe that people’s limits are in flux and change over time.
Caregiver Agreements
- Caregivers commit to attending Saturday clinical programming. For every Saturday their teen is at The Farmhouse, the clinical programming starting at 9:30 AM and ending at 7:30 PM. Whole family wellness begins with the entire family learning and practicing skills one-mindfully together, setting aside distractions. Services include the DBT Skills Multi-Family Group, the Relationship Education & Enhancement Program, the Parent Effectiveness Training, the Nutritional Psychiatry and Culinary lab, and family therapy, parents commet to being presetnf or all components of treatment.
- Caregivers commit to practicing all the skills taught throughout the week, at home and in other settings to model to their teen that changing ineffective habits is possible. This may look like modeling taking a non-judgmental stance when observing and describing behavior, leading with perspective taking, and practicing benign interpretations of family members’ behaviors by giving the other person the benefit of the doubt.
- Caregivers agree to throw themselves fully into learning to the skill of validation, understanding that validation does not equal approval or agreeing with their child or partner. Validation is a skill that helps others feel heard, lowers intense emotions, and provides the requisite balance to requests for change. leads to less emotion dysregulation Validation is the primary method by which a parent helps neurologically tune their child.
- Caregivers agree to follow the treatment plan recommendations of the treatment team, which may mean adding their own individual and/or couple therapy, if that is required to help optimize balance, flexibility and psychological safety within a family system.
- Caregivers commit to using skills when frustrated with Compass Staff, agreeing to observe and describe the behavior or concern in a non-judgmental way, describing the impact the behavior has had on them, and asking for a specific behavior change request. Caregivers may bring such requests and feedback to the clinical director. Said another way, caregivers agree to speak up and not stew in frustration.
DBT Assumptions about Clients
- Clients are doing the best they can.
- Clients want to improve.
- Clients need to do better, try harder, and be more motivated to change.
- Clients may not have caused their own problems, and they need to solve them anyway.
- The lives of clients are unbearable as they are currently being lived.
- Clients must learn new behaviors in all relevant contexts.
- Clients cannot fail in therapy.
- DBT Team members need support.
DBT Assumptions about Therapy
- The most caring thing a DBT provider can do is help people solve their problems.
- Clarity, precision, and compassion are of the utmost importance in solving problems.
- The therapeutic relationships is a real relationship between equals.
- Principles of behavior are universal, affecting DBT providers no less than clients.
- DBT providers can fail.
- The treatment can fail even when DBT providers do not.
Dialectical Behavior Therapy Skills Group
Three times per week, residents engage in a 90-minute DBT skills group. This group is structured like a class, in that it is didactic in nature, even though skill leaders do often teach in an experiential and engaging way. Owing to an average 30-day length of stay in our program, the curriculum for the DBT skills group does not include the full 24-week DBT skills curriculum that is typically delivered in outpatient therapy. Rather, there are 12 lessons taught that cover the Distress Tolerance and Emotion Regulation modules. The other modules of Mindfulness and Interpersonal Effectiveness are covered in other elements of the programming. Each resident gets focused time to review homework followed by presentation of new material each week. The purpose of the skills group is to learn and intentionally practice coping skills. The skills are then used to help residents address problems in other parts of the program. Research supports the use of DBT for Adolescents (i.e., McCauley et al., 2018; Miller, Rathus and Linehan, 2007).
Interpersonal Effectiveness Group
Residents will engage in an interpersonal effectiveness group once a week for 60-minutes. In this group, residents will participate in four lessons, two of which are from the DBT skills curriculum, and the other two are derived from the Unified Protocol and graciously shared with our program Children’s Hospital Colorado Adolescent Partial Hospitalization Program. This group has a didactic component and is heavily experiential with communication practices each group. Residents will learn how to prioritize their objectives, self-respect and relationship goals, and effective communication strategies to achieve them. Research supports increasing communication skills for adolescents as way to yield positive mental health outcomes (i.e., Kim & White, 2018).
Mindfulness & Mindful Self-Compassion
Residents begin each day with 30 minutes of mindfulness and mindful self-compassion. This group consists of experiential exercises followed by a brief didactic on the particular practice. Following the practice, residents will set a goal for the day and at the end of the day, they review their goal in another mindfulness group. The mindfulness curriculum is derived from the mindfulness module in DBT skills and the mindful self-compassion curriculum is derived from The Self-Compassion Workbook for Teens (Bluth, 2017). Research supports the use of Mindfulness with adolescents (i.e., Black, 2015; Burke, 2010).
Individual Skills Coaching
Directly after individual therapy, residents will engage in individual skills coaching twice-weekly for 60-minutes. During individual skills coaching, residents work on requisite behavioral rehearsal of skills identified during individual therapy.
Therapy Interfering Behavior Protocol
Treat TIBs like a problem to solve and assume the resident is motivated to solve their problems.
1. Define the interfering behavior
ex: Client refusing to attend group.
2. Conduct a Behavior Chain Analysis to assist client and guide to generate a hypothesis to TIB.
-
- Let go of “why” the client is refusing and focus on what led to the refusal. When we review the function of their behavior, it will give us more of an understanding as to “why” they are engaging in this behavior.
3. Adopt a problem-solving plan and gain resident’s commitment to implement solutions and rate their willingness on scale of 1-10
-
- Inform primary therapist of:
-
- Residents TIB
- Solutions Identified
- Level of willingness to implement solutions
-
- Inform primary therapist of:
Egregious Behavior Protocol
Clinicians Posting Egregious Protocol in the Comm Log
Using the following template:
Related incident Report Date:
Related Com Log Summary (hyperlink):
Describe Egregious Bx:
Previous Efforts to address Target Bx:
Document in the Thread Each Step as its Targeted
Step 1: Chain Analysis
Does the resident have a missing skill that is a prequisite skill to be able to complete this step? If yes
-
-
- Response Plan:
- Milieu Intstructions & Resident Feedback:
- Follow-up: Writer will post updates daily in this thread until the Egregious Protocol has been lifted.
-
Step 2: Reestablishment Commitment
Does the resident have a missing skill that is a prequisite skill to be able to complete this step? If yes
-
-
- Response Plan:
- Milieu Intstructions & Resident Feedback:
- Follow-up: Writer will post updates daily in this thread until the Egregious Protocol has been lifted.
-
Step 3: Solution Analysis & Behavior Rehearsal
Does the resident have a missing skill that is a prequisite skill to be able to complete this step? If yes
-
-
- Response Plan:
- Milieu Intstructions & Resident Feedback:
- Follow-up: Writer will post updates daily in this thread until the Egregious Protocol has been lifted.
-
Step 4: Corrects the harm caused / Over Correction
Does the resident have a missing skill that is a prequisite skill to be able to complete this step? If yes
-
-
- Response Plan:
- Milieu Intstructions & Resident Feedback:
- Follow-up: Writer will post updates daily in this thread until the Egregious Protocol has been lifted.
-
Step 5: Egregious Protocol Lifted
Treatment Outcomes
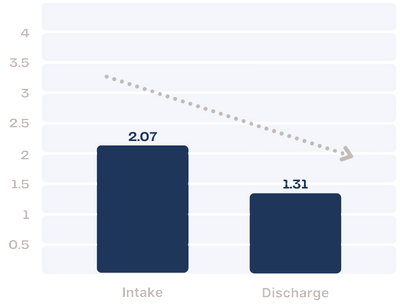
PHQ-A
The PHQ-A is a 9- item measure that assesses the severity of depressive symptoms in children ages 11–17. It is administered weekly and instructs the adolescent to report their symptoms over the past seven days.
On average, Farmhouse residents in 2023 decreased from the “moderately severe” range to the low end of the “moderate” range over the course of treatment.
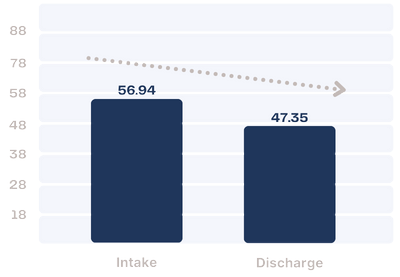
GAD-7
The GAD-7 is a self-report questionnaire designed to screen for severity of symptoms associated with generalized anxiety disorder.
On average, Farmhouse residents in 2023 decreased from the “moderate anxiety” range to the “mild anxiety” range over the course of treatment.
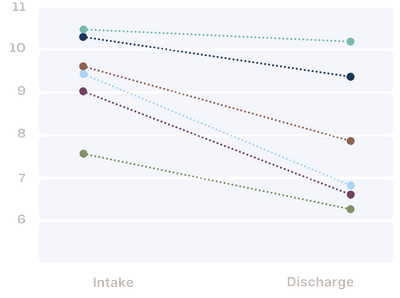
SCIM
The SCIM is a measure of “healthy” and “disturbed” identity. Increased scores on the SCIM are also associated with emotion dysregulation and depression.
Farmhouse residents in 2023 report decreased identity disturbance at the end of treatment.
BSL-23
The BSL-23 is a 23-item self-rating instrument for specific assessment of borderline personality disorder (BPD) symptoms, including affect instability, suicidal behavior, self-harm and dissociation. The BSL-23 also assesses self-criticism, problems with trust, emotional vulnerability, proneness to shame, and emptiness (Bohus, et. al., 2007).
BPD symptomology for Farmhouse residents in 2023 moved from the “high” range to the “moderate” range over the course of treatment (Kleindienst, et. all., 2020).
DERS-SF:
OVERALL
The DERS-SF assesses emotion regulation problems among adolescents and adults.
Difficulties with Emotion Regulation among Farmhouse residents in 2023 moved from the “Severe” range to the “Moderate” range over the course of treatment.
SUBSCALES
Awareness
higher scores indicate greater inattention to emotional responses
Non-Acceptance
higher scores indicate greater inattention to emotional responses
Strategies
Higher scores indicate less access to emotion regulation strategies, and greater beliefs that there is little a person can do to effectively regulate their emotions after becoming upset
Impulsivity
higher scores reflect greater struggles to control behavior when upset
Goals
goal-directed behavior, higher scores indicate problems concentrating and accomplishing tasks while experiencing negative emotions
Clarity
reflects extent to which individuals are unclear about which emotions they are experiencing; higher scores indicate greater difficulty identifying emotions that they are experiencing
Satisfaction Surveys
Average resident rating of overall satisfaction with the Farmhouse residential program:
4.15 out of 5
%
Average resident rating of Individual Therapy:
4.2 out of 5
%
Average caregiver rating of overall satisfaction with the Farmhouse residential program:
4.5 out of 5
%
Average caregiver rating of Family therapy:
4.7 out of 5
%
86% of residents agree or strongly agree that they “better at handlinglife” as a result of the Farmhouse residential program.
- 86%
89% of caregivers strongly agree that they would refer another family to the Farmhouse for Residential treatment.
- 89%
What Graduates are Saying…
I am able to go home and use the stills I have learned to tolerate distress, bullying, discrimination, invalidation, and self-doubt. Because of this, I KNOW that I will be able to build and live my life worth living, which is something I never really believed was possible before I came to Compass.
The most helpful thing during my stay at the Farmhouse was the compassion I received from the staff. When I was really struggling (self-harming, making an attempt, or having a panic attack), the staff were almost always very kind, understanding, and patient with me. They would wait for me to calm down, offer skills, or just sit there and listen, and I really appreciated it. I haven’t had the best experience with mental health treatment, so being treated with kindness and empathy helped me reframe my thoughts and beliefs around treatment and realize that not all treatment is bad and harmful.
This program has truly been so wonderful for me and my Family, I cant thank you all enough. I am really blessed to have had the experience of being here. Thank you!!! 🙂
I’m so glad I’ve come here staff are amazing and i feel so welcome, i can see the growth with myself and my family.
I Love the Farmhouse and all of the staff here. I am so lucky to have gotten this experience and treatment.
Why would our graduates recommend the Farmhouse to someone in need…
Most of the staff is phenomenal, the way they do things here is great and really prepares us for going back into the world.
Because this treatment is incredably effective for so many different reasons. The staff all pay so much attention, and put so much effort into helping the residents, and the therapists are truley invested in their clients lives, and the outcome of their treatment. The staff here are motivated to do the work, which in turn motivates the kids. This program is amazing!!!!!!!!!!!!!!!!!!

