Treatments
Treatments
A Compassionate Approach. An Evidence-Based Track Record.
“Dialectical” is an elegant way of saying that two opposing things can be true at the same time. You can be happy and sad about the same thing within the same moment. Dialectics help us to lean away from “right” and “wrong” and move towards a synthesis. It’s okay to be happy. It’s okay to be sad. It’s even completely okay to feel happy-sad!
Dialectical behavioral therapy was developed by Marsha Linehan. Recognized by TIME Magazine (July 2018) as one of the most important scientists of our time, Dr. Linehan created the most effective treatment to date for pervasive emotion dysregulation and symptoms of chronic suicidality and self-harm. Her approach was revolutionary – pulling from her study as a Zen student, compassionate – weaving in from her own experience a psychiatric patient, and ultimately effective – with 42 randomized controlled studies replicated around the world.
Through a delicate balance of skills training, individual treatment, in-the-moment coaching, and team-based consultation, DBT equips patients with five types of behavioral skills:
- Mindfulness: the practice of being fully aware and present in this one moment
- Distress Tolerance: how to tolerate pain in difficult situations, not change it
- Interpersonal Effectiveness: how to ask for what you want and say no while maintaining self-respect and relationships with others
- Emotion Regulation: how to change emotions that you want to change
- Middle Path: how to move away from black & white, all or nothing thinking and see the situation from multiple valid perspectives.
The goal is not only to help people survive major crises, but to develop the skills and behaviors that allow them to enjoy “lives worth living.”
DBT-Linehan Board of Certification™: The Gold Standard
Like so many wellness-related words and phrases, “DBT” can refer to many things. Unfortunately, many of them have little to do with the evidence-based protocols developed by credentialed practitioners. That’s why Compass works exclusively with the DBT-Linehan Board of Certification,™ to maintain the highest standards of clinical excellence in the practice of DBT.

What it Means to Be a DBT-Linehan Board of Certification, Certified Program™
Compass Behavioral Health was the first DBT-LBC, Certified Program™ in California.
Achieving this certification is the result of a rigorous 12-month process that includes:
- Individual certification for the team leader
- A complete review of all protocols for research adherence
- Patient interviews for DBT skills knowledge
- Observation and adherence coding of a DBT skills training group
- Observation and adherence coding of the DBT Consultation Team
- Chart reviews for treatment adherence and measurable outcomes being tracked
DBT Adherence: What’s the Big Deal?
Families often come to us after doing their own research and reading impressive statistics about the efficacy of DBT treatment. It’s important to note that these results were achieved by clinicians meeting required standards of DBT proficiency and competence. Unfortunately, not all practices billing themselves as “DBT” follow these standards. In 2011, the Substance Abuse and Mental Health Administration issued a strong warning to the United States Congress regarding programs being marketed as “DBT” that lacked adherence, achieving poorer outcomes than those attained in the research. That’s why formal DBT certification and program accreditation have been put into place.
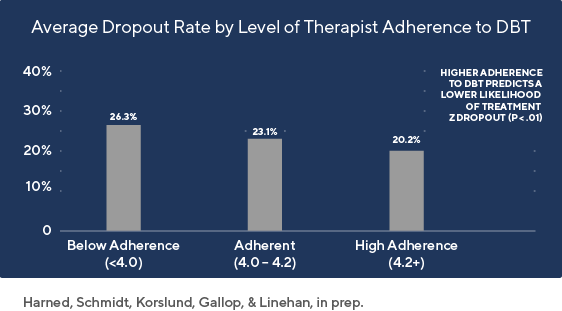
ADHERENCE TO DBT REDUCEDS TREATMENT DROPOUT
Why Certification Matters
- DBT is a treatment that saves lives. Consumers, insurance companies and state regulatory agencies have long petitioned DBT founder Dr. Marsha Linehan for a means of identifying credible DBT therapists. Certification by DBT-LBC was created to answer those requests.
- As developed by Dr. Linehan, DBT is recognized by the United States Substance Abuse and Mental Health Services Administration to be an evidenced-based practice.
- DBT-LBC Certification is the only DBT Certification credential recognized by Dr. Linehan.
- DBT-LBC provides easy on-line access to listings of DBT-LBC Board Certified Clinicians and Programs to clients in great need.
- Board Certification in DBT, like in all healthcare professions, shows a clinician’s willingness to be reviewed by experts and held to high professional standards.
So-called “DBT” programs that lack adherence and merely “adapt DBT” rather than “adopting DBT” can put patients at risk and create heightened liability for practitioners. When evaluating whether a DBT program is right for your family, look for the DBT-Linehan Board of Certification gold standard.
- With thanks to Roy Krawitz, MBBCH, FRANZCP, MNZAP Consultant Psychiatrist, Waikato District Health Board and Honorary Clinical Senior Lecturer, Auckland University.
What We Treat
ADD & ADHD
Attention-Deficit Disorder and Attention-Deficit/Hyperactivity Disorder involve significant difficulty maintaining attention and restricting impulsive urges. These disorders may cause impairment in educational and occupational settings, significant personal distress and shame regarding difficulty completing tasks in a timely manner, and interpersonal/familial conflict.
Anger
Anger management disorders include displays of aggression towards self or others, destruction of property, intense physiological responses to triggers such as clenching of the jaw and hands, and thoughts of committing harm. Individuals suffering from anger may experience may interpret situations as overly threatening and believe they must respond in this way to protect themselves from harm. These can result in deeply dysfunctional interpersonal relationships, a sense of helplessness, and even physical injury to oneself and others.
Anxiety
An expectation of a future threat, anxiety activates the body and prepares it to respond. While some anxiety is normal, high levels of persistent anxiety can lead to fear of new situations or people, difficulty with changes in routine, avoidance of challenging situations, and reduced performance on tests and other known activities.
Bipolar Disorder
Bipolar Disorder is marked by “highs and lows” that may include periods of depression and periods of elevated mood (otherwise known as “mania” or “hypomania”). Changes in mood may appear several months apart or may seem “rapid cycling” and occur as often as every other day.
Borderline Personality Traits
Individuals with Borderline Personality traits may feel “dysregulated” for long periods of time and report difficulty in controlling their own emotional states, with periods of anger, anxiety, fear, guilt/shame, and sadness possibly lasting far longer than expected by others. Individuals with Borderline Personality traits are at an increased risk of experiencing suicidal attempts and thoughts. Additionally, self-harm is often present, including cutting the skin, burning, and other acts which serve to intentionally damage their bodies.
Depression (including suicidal and self-harm behaviors)
Depression involves persistent sadness that is experienced throughout the day. It includes a pattern of feeling “down” or sad for longer than two weeks, lack of interest or pleasure in activities that used to be preferred, thoughts of suicide, feeling worthless, and changes in sleep and appetite. Depression can have significant impacts across several areas in life, including self-esteem, social networks, school, jobs, and hobbies.
Eating Disorders
Eating disorders present significant challenges to everyday life. Anorexia Nervosa is a condition in which an individual restricts their eating and displays an inability to maintain a healthy body weight. Fears of gaining weight are often present, often to the point of obsession. Bulimia Nervosa is a condition marked by overeating to the point of feeling physically ill. Food eaten is removed from the body by vomiting/purging or use of laxatives. This cycle of binging and purging creates an intense need for the individual to regulate what they eat and may contribute to life-threatening physical conditions.
Family Systems Problems
Each member of a family has unique relationships with other family members. Problems occur when communication feels ineffective in motivating others in the family towards action viewed as necessary to maintain family structure. Problems may be related to topics such as use of language (or specific words that feel triggering to others), household responsibilities such as chores and finances, failure to adhere to pre-determined family rules or lack of structure, parenting, and boundaries.
Impulsivity
Includes risky actions made on the spur of the moment without planning or thought of consequences. Examples include difficulties regulating spending, thrill-seeking behaviors, chronic overeating, substance use, difficulties regulating one’s own comments during conversation, theft, and poor decision-making.
Low Self-Esteem
Self-esteem is a person’s measure of their own sense of self-worth. Low levels of self-esteem are a risk factor for sadness and depression.
Parenting Issues
Difficulties in parenting may include a child displaying physical violence towards themselves or others, lying, substance abuse, and viewing parents as a lack of authority in the household. Additionally, disagreements between parents can cause significant distress both in the family and with each other.
Post-Traumatic Stress Disorder (PTSD)
PTSD can develop after an individual experiences or witnesses a life-threatening event such as sexual assault, physical threats to well-being, death, accidents, natural disasters, or other highly stressful events. Individuals with PTSD also often experience difficulties with sleep and concentration, increased startle response, feeling the need to be on guard and alert at all times, and persistent negative thoughts.
Misophonia
Misophonia is a condition where intense negative emotions are triggered by specific sounds. Such sounds may include chewing, drinking, sniffing, talking, nail clipping, creaking, tapping, or repetitive sounds. Sufferers will attempt to avoid sound sources, which can produce significant negative impacts in attention, productivity, and social relationships.
Obsessive-Compulsive Disorder (OCD)
OCD-sufferers experience intense urges to check, fix, or focus on a situation or object repeatedly. This condition is often associated with high levels of anxiety if such actions cannot be completed in a pre-determined time or to adequate satisfaction. OCD symptoms often cause delays in completing tasks and marked impairment in day-to-day functioning.
Social Skills Deficits
Individuals with social skills deficits find it difficult to form relationships and communicate their wants or needs, which can also result in frustration, anger, and disrupted relationships.
Substance Abuse
Individuals suffering from substance abuse may feel dependent on continued use despite the negative consequences of use and may experience difficulty regulating the frequency that they use such substances. Further, some substances eventually create triggers for negative interactions with friends and family. Continued use may lead to life-threatening conditions.
Trichotillomania & Excoriation
Trichotillomania is a disorder involving the compulsion to pull hair out from the scalp, eyelashes, arm, or other parts of the body. Excoriation is similar but involves excessive picking of one’s own skin to the extent of causing damage. Although some individuals report conscious control of their desire to pick, others find that they are unaware that they have picked until several hours later. As it feels difficult to be aware of when such picking is taking place, such individuals report high levels of frustration and inability to change this behavior.
Other Evidence-Based Therapies
While Compass has a primary focus on the development and practice of DBT-based protocols, we also combine DBT
with other evidence-based treatment protocols including:
Acceptance and Commitment Therapy (ACT)
Acceptance and Commitment Therapy (ACT) helps individuals identify their core values and work to reach goals based on those values despite the presence of mental health symptoms. Individuals learn skills that assist in reducing avoidant coping styles and increase commitment to making changes. ACT is an evidence-based psychotherapy that has been shown to be effective for treating various types of anxiety and depression.
Behavioral Activation
When people get depressed, they tend to withdraw from life. This can mean abandoning their routines, disengaging from their environment, and pulling away from the people in their lives. Over time, this avoidance can create a vicious downward spiral as depressed people lose opportunities to enjoy pleasant experiences, which exacerbates their depression.
Behavioral Activation is a practice designed to reverse this cycle. We work with patients to increase their exposure to rewarding experiences. There are various versions of Behavior Activation that we can choose to employ depending on the individual patient, with a slightly modified emphasis on activities, problem solving skills, and identifying processes.
Cognitive Behavioral Therapy (CBT)
CBT is a short-term, goal-oriented psychotherapy treatment that takes a hands-on, practical approach to problem-solving. CBT teaches individuals skills to change patterns of thinking or behavior that are contributing to their difficulties.
CBT-E
CBT-E is the abbreviation for “enhanced cognitive therapy” and consists of a highly personalized treatment for those with eating disorders.
In practice, CBT-E generally involves an initial assessment appointment followed by weekly treatment sessions over the course of 20 weeks. With people who are seriously underweight, treatment needs to be longer, often requiring 40 weeks of treatment sessions.
CBT-E has four stages:
- In Stage One, the focus is on gaining a mutual understanding of the eating problem and helping patients stabilize their eating patterns.
- In Stage Two, we review progress and make plans for the main part of treatment.
- Stage Three consists of weekly sessions focused on the processes that are maintaining the person’s eating problem
- In Stage Four, the emphasis shifts to the future. There is a focus on dealing with setbacks and maintaining the changes that have been obtained.
Some months after treatment has ended, a review session is held to catch up on the patient’s progress and address any new issues or concerns.
Cognitive Processing Therapy (CPT)
CPT is based on Cognitive Behavioral Therapy and the assumption that thoughts and emotions directly affect one another. CPT involves helping clients identify their beliefs that have shifted and are keeping them stuck with post-traumatic stress and it teaches them skills to evaluate and modify these beliefs to make them less extreme.
Executive Function Coaching
Executive Function skills are self-management skills that help people manage their emotions, focus attention, organize and plan their work and time, and reflect upon and revise their tactics as circumstances change. As the demands of school increase each year, having well developed Executive Function skills becomes critical in order to achieve academic success. Students who have been diagnosed with ADHD and/or learning differences often have Executive Functioning challenges.
Exposure Response Prevention
Exposure Response Prevention (ERP) is a therapy designed to treat obsessive-compulsive disorders through exposure to upsetting or “triggering” situations.
Exposure therapy starts with confronting items and situations that cause mild anxiety. After the patient starts to feel comfortable with exposure, we move on to more difficult exposure exercises. ERP is often combined with Cognitive Behavioral Therapy (CBT) to help patients develop a more in-depth understanding of their thought processes and behaviors.
Initially, many patients feel intimidated by the idea of being asked to face their fears. However, we’ve generally found that patients don’t find exposure exercises nearly as difficult as they imagined. The therapy is designed to be gradual and compassionate to patients as they engage in the process of coming face to face with the sources of their obsessive thoughts and compulsive responses.
Family Therapy
At Compass, the entire family is the focus of treatment. This approach ensures that every member of a family in distress receives the support, healing, and education to move forward to a state of well-being. Sessions will include meeting with a licensed and trained family therapist who will guide you through the essential steps of recovering your family in the middle of the crisis.
Mastering Anxiety and Panic
MAP-A is a type of exposure therapy that includes strategies and techniques to help individuals deal with panic disorder and agoraphobia. The main function of the treatment involves corrective learning and prepares adolescents to face agoraphobic situations and physical symptoms of panic from a new perspective.
Mindfulness
Mindfulness is an evidence-based practice designed to manage stress and improve daily functioning. Practicing mindfulness can be defined as connecting with one’s inner experience of the present moment with acceptance and curiosity.
Mindfulness Based Cognitive Therapy (MBCT)
MBCT is designed to help people who suffer repeated bouts of depression and chronic unhappiness. It combines the ideas of cognitive therapy with meditative practices and attitudes based on the cultivation of mindfulness.
Motivational Interviewing (MI)
MI is an important prelude to therapy work, in which the therapist becomes a helper in the change process and expresses acceptance of the patients. Although some patients can continue change on their own, others require more formal treatment and support over the long journey of recovery.
Mindful Self-Compassion
It is vital for adolescents to learn the difference between making a bad or harmful decision and being a “bad person.” Through self-compassion skills training, we guide our patients and families toward acceptance of self, in good times and bad, without judgment.
Prolonged Exposure Therapy (PE)
PE is a specific type of exposure therapy that is used to treat post-traumatic stress disorder. PE is a time-limited, evidence-based treatment that works for most people and ultimately helps individuals live the lives they want to live without being controlled by their trauma symptoms.


